Brainstem cavernoma with two hemorrhages
20 year old women with spinal cord ca
- Update Time:2023-05-22 16:37:36
- Our Patients
"This surgery was different, this time we took out the whole lesion". This was during the second week after Professor Bertalanffy had successfully removed Rachel's extremely dangerous intramedullary cavernoma in the thoracic spinal cord. The cavernoma in her thoracic spine had been with her for two years, a ticking time bomb ready to off anytime. After two bleedings, it already had eaten away at Rachel's ability to move and had caused incontinence. As the disease progressed rapidly, the family's otherwise happy life was plunged into darkness. Although rehabilitation therapy had restored some of her mobility, the family was in constant worry about a third bleeding that could trap the child in a wheelchair forever.
Now, looking at the girl who just underwent successful surgery, she seemed to not worry about being paralyzed anymore. Professor Bertalanffy and the parents knew that this success didn't come easy. This was but the first step in Rachel's new life, now that she was liberated from the thoracic intramedullary cavernoma. Listening to the professor's advice, she took the courage and energy to keep exercising and to carve out a better future. “She should work hard, work hard doing exercises, then she will notice”.
How long does it take from being a healthy person to being permanently paralyzed on one side? Maybe just five minutes. One of our cases involved a young girl. After continuously working overtime, she developed "a tearing pain in the back". After just five minutes, she was completely paralyzed. Motor function of her upper limbs was partially recovered after surgery, but the doctor had to inform her with regrets, that even with active rehabilitation, the paralysis below her chest would not recover. For the rest of her life, she would be tied to a wheelchair, owed to the extremely dangerous cavernoma in her thoracic spine. In contrast to the outcome of this poor girl, Rachel considers herself lucky when she looks back at at her journey.
How dangerous is an intramedullary thoracic cavernoma?
After two hemorrhages, the young girl is bound to a wheelchair.
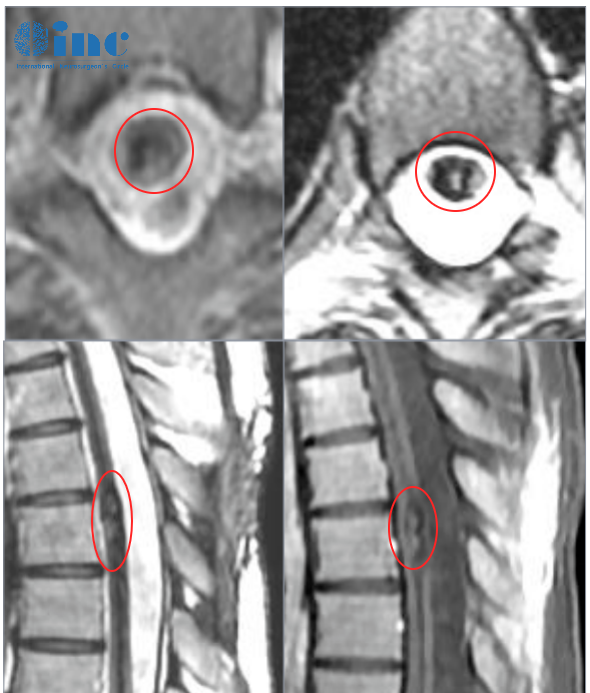
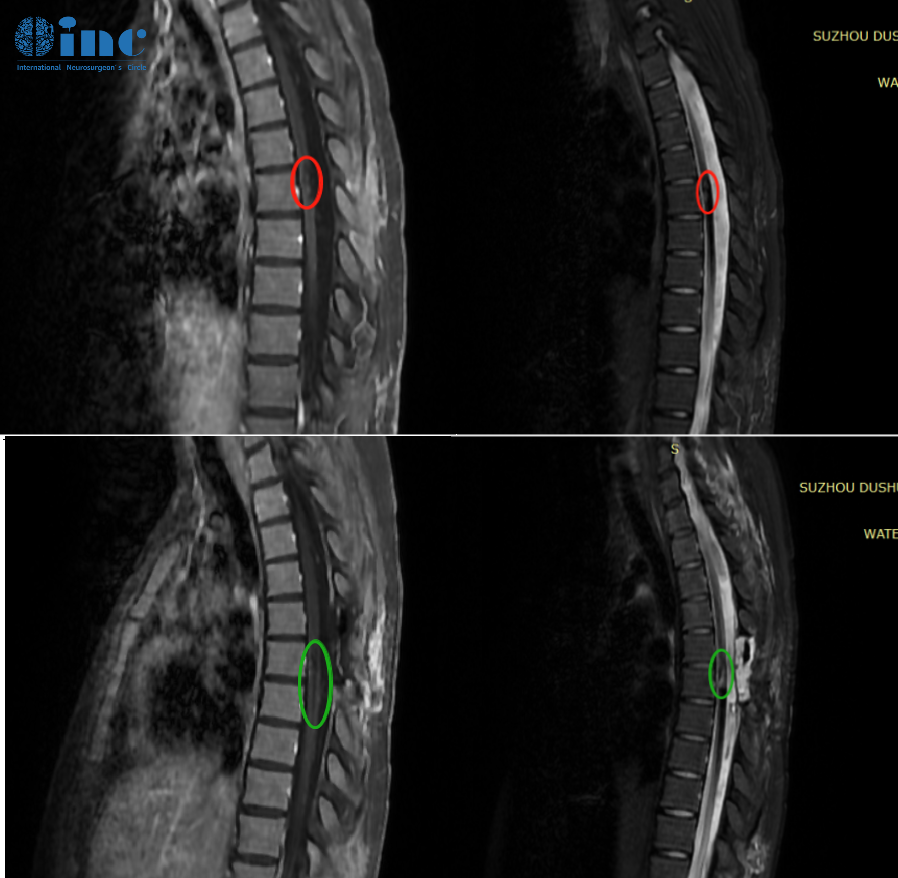
Two years earlier, Rachel had just started college when she noticed a slight back pain after doing her regular exercises. She first thought it was muscle pain and that it would recover after a few days of rest. But after two days, her pain hadn't improved, instead she now developed a weakness in her lower extremities. Sensing that something was wrong, Rachel rushed to the doctor to have her examined. The results she got were crushing. Her MRI showed a hemorrhagic lesion within the thoracic spinal cord. Her doctor immediately suspected a cavernous hemangioma. From then on, her disease progressed rapidly, as Rachel experienced difficulties urinating, and both her lower limbs grew even weaker. Another MRI scan confirmed the cavernoma at level Th6 of her thoracic spine. After considering the deep location of the lesion on the ventral side of the spine, the doctor deemed surgery too risky. Just a slight mishap during the procedure, and Rachel would be permanently paralyzed. Conservative treatment was the only viable option to recommend. After a period of conservative treatment, Rachel's weakness in both legs improved a bit, and she was able to walk on her own again.
But the improvement did not last long. A second bleeding struck Rachel again after one year, leaving her numb in her right leg. An examination confirmed the second bleeding.
Within two days, her symptoms became much worse, with loss of motor function in both lower limbs and incontinence. In order to alleviate her symptoms, doctors performed a partial laminectomy to enlarge the space for the spinal canal, a standard decompression technique, but they did not remove the cavernoma. As they witnessed their daughter's condition deteriorate further and further, the parents decided to seek out better treatment options.

The clinical symptoms of an intramedullary cavernoma and their severity depend on several factors, such as the location of the cavernoma, the volume as well as the number of hemorrhages, the degree of injury to the affected segment of the spinal cord and more. Accordingly, symptoms can vary wildly, but mainly include pain caused by local nerve compression, sensorimotor deficits and sphincter disorders. The hemorrhage of Rachel's cavernoma had already caused lower limb dysfunction and incontinence. Nobody dared to imagine what yet another bleeding could cause if she was not operated.
During the two-year course of Rachel's disease, the family had consulted with numerous doctors, trying everything for her to undergo surgery. But the answer they received again and again was: Surgery was too risky. Operating within the spinal cord was simply beyond the capability of most doctors. The spinal cord is the major pathway that connects the brain and the peripheral nerves outside the central nervous system. It is densely populated with 31 nerve ganglia (clusters of nerve cell bodies) and four motor nerve tracts that originate in the brainstem. Manipulating these structures just a tiny bit too much, or excessively using electrocoagulation to stop bleeding during the surgery (otherwise a standard technique) can cause spinal cord infarction. Before the surgery, Rachel already suffered from serious symptoms. If the surgery was not performed well, she might never be able to stand up again for the rest of her life.
What would happen if no surgery was done? What would await her is unpredictable. Another re-bleeding could cause permanent paralysis.
And what would happen is surgery was done? If the surgery was not done well, the outcome might be all the same. But every time they looked at her cheerful daughter with the huge smile on her face, the parents were convinced that this could not be the only outcome. So they continued to look for a surgeon who could safely perform the surgery.
One of the world's leading neurosurgeons visiting China
Successful removal of the "ticking time bomb"
During his one-month visit to China in 2022, Professor Bertalanffy successfully performed nearly 30 complex surgeries, including four surgeries in the spinal cord, one of which involved a tumor measuring 14 cm from the brainstem into the spinal cord. The patient recovered well after the surgery and is now able to walk again and hold objects in his hands.
Upon receiving the news of Professor Bertalanffy's return to China in 2023, Rachel's parents hope to save their daughter finally seemed to materialize. They immediately contacted INC for a remote consultation with Professor Bertalanffy. How high is the risk of the surgery? What can we expect of post-operative recovery?

"Every time I operate on a cavernoma of the brain or spinal cord, I intend to remove it completely.
As far as complications go, I have a very low incidence rate with respect to spinal cavernoma.”
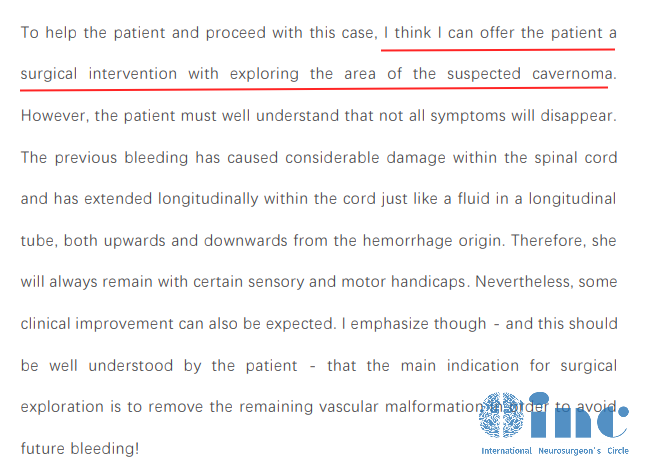
INC's medical team collected and translated all the relevant files of Rachel's case history. After having studied Rachel's case, Professor Bertalanffy summarized: "The previous bleeding has caused considerable damage within the spinal cord and has extended longitudinally within the cord just like a fluid in a longitudinal tube, both upwards and downwards from the hemorrhage origin." He could offer Rachel the surgery, and while the surgery would clinically improve her pre-existing symptoms to some extend, not all symptoms would disappear. The main goal of the surgery was to remove the remaining vascular malformation in order to avoid a future re-bleeding that would cause even more severe symptoms. He could safely remove the cavernoma in Rachel's thoracic spine.
After reading Professor Bertalanffy's reply, Rachel's parents burst with excitement. They finally found a doctor who could do the surgery safely. They understood that recovery would take a long time and that the goal of the cavernoma resection was to avoid another bleeding. As this could happen at any time, they decided to hurry up and take advantage of the opportunity. So they applied for Professor Bertalanffy's surgical demonstrations scheduled for the spring of 2023.

Spring 2023 surgical demonstrations by Professor Bertalanffy - Resection of a thoracic intramedullary cavernoma
Following the consultation with Professor Bertalanffy, the family was well informed about the benefits of the surgery. But when they saw the professors confident and determined demeanor with their own eyes and heard his evaluation of the surgery, the family's minds were set at ease. Rachel trusted that in his skilled hands, she would overcome her disease and get back on her feet. "Thank you, professor! Thank you!See you tomorrow!" ...…The purpose of the surgery is to remove the existing cavernoma, because a future bleeding is guaranteed to happen, causing even more symptoms and possibly the complete loss of motor function. Now that we completely take out the cavernoma, rehabilitation exercises are important to increase muscle strength and to relieve symptoms. The main goal is to take out the cavernoma and to prevent future bleedings from causing more damage. Judging from the MRI images, injury to the spinal cord is not very serious, so there is a very good chance that her symptoms could be alleviated. Simple rehabilitation exercises could be started immediately after the surgery, and then full mobilization exercises two to three weeks later.
- Professor Bertalanffy’s pre-operative briefing
Thanks to the intra-operative electrophysiological monitoring, the surgery could be safely performed. In cooperation with his Chinese colleagues, Professor Bertalanffy meticulously and gently peeled of the lesion layer by layer from within the thoracic spine.
The primary goal of the surgery was to preserve the function of the spinal cord by safely separating the cavernoma from it, while resecting as much as possible. It was of utmost importance, to gently handle the instruments and to absolutely minimize traction on the spinal cord, protecting it from the beginning to the end of the surgery. The spinal cord was incised at the posterior median sulcus. Damage to important nerves was avoided with the help of intra-operative electrophysiological monitoring; in the end, the surgery was successful, the cavernoma was safely removed from Rachel's spinal cord.
Rachel's parents had been waiting the whole time outside the operating room. When they saw Professor Bertalanffy leaving, they rushed up to him to ask how the surgery went. The professor showed them picture he had taken during the surgery, pointing out the location from where he had removed the cavernoma. "It's a clean resection!"As Rachel's parents received the good news, a huge weight had been lifted off their shoulders.

On the day after the surgery, Rachel was resting in the ICU. "I feel so lucky to have met Professor Bertalanffy", she exclaimed, this 20-year-old girl already being able to communicate normally. She felt extremely fortunate to get a chance at this surgery. About the recovery of Rachel's symptoms, Professor Bertalanffy said that rehabilitation was very important! Rachel should slowly increase exercises, then the symptoms would slowly get better!
On the fifth day, Rachel already felt very good, the muscle strength in both her legs was better than before the surgery.
During our most recent follow-up one month after the surgery, Rachel was able to get out of her bed and walk around freely. Her pre-operative symptoms had subsided.
As Professor Bertalanffy had explained to her during his last visit on her ward, the young girl would have to pluck up all her courage and energy marching into the future. We will continue to follow up on Rachel's recovery and wish her nothing but the best for her future.
Monday Jul 29, 2024
Contact: inc-office@inc-sg.net


